|
Medicine often has side-effects or unintended consequences that are more harmful than the original disease. Medical anthropology in
general and the illness–disease distinction in particular has been introduced into historical
Jesus research with the intent to protect it from medicocentrism and thus to offer ways of comprehending sickness and healing in the world of Jesus and his first followers without distorting these phenomena by imposing the biomedical framework onto the texts. In particular the illness–disease distinction is used for making sense of healing accounts whilst claiming to cross the cultural gap. Based on an analysis of the illness–disease distinction in medical anthropology and its use in historical Jesus research this article suggests that instead of protecting from ethnocentrism this distinction actually increases the risk of ethnocentrism and consequently distorts in many instances the healing accounts of the New Testament.
It is remarkable how frequently medical anthropology in general and the illness–disease distinction in particular are nowadays invoked in New Testament scholarship to facilitate ethnocentric-free cross-cultural interpretation. John Pilch suggests that insights from medical anthropology in general and the illness–disease distinction in particular will facilitate ‘cross-cultural communication, understanding, and interpretation’ (2000b:130). He maintains that concepts such as illness and disease, healing and curing ‘have eliminated or at least minimized the risk of falling into medicocentric interpretations’ (2010:147). John Dominic Crossan (1994:80) argues that insights from cross-cultural anthropology, such as the ‘basic distinction’ between illness and disease in medical anthropology, ‘prevent us from projecting some current American presuppositions back into the ancient Mediterranean world’. For Eric Eve (2002:353), Kleinman’s ‘careful distinction’ between illness and disease is devised for cross-cultural comparison and may be applicable to the ancient Mediterranean and therefore also to the gospel accounts. Richard Horsley claims that reductionist psychological explanations can be avoided when stories about demon possession are interpreted by means of critical medical anthropological categories. In particular the illness–disease distinction gives him the license to treat cases of demon possession as instances of political-economic exploitation whilst exorcisms are seen as events of opposition to imperial rule (see 2008b:43). In his words, ‘critical medical anthropologists have recognized that illness often involves particular relationships of power, domination, and deprivation’ (2008a:85). If these insights were true, they would provide powerful interpretive tools for understanding Jesus’ healings as historical acts whilst ethnocentric misinterpretation would be avoided. However, the truth is that taxonomic schemes, however necessary and indispensable for research, can also be the source of error and obfuscation when dealing with nature, history or reality. The first step in determining whether these claims are valid would be to ask how the distinction functions in medical anthropology and whether it in fact is a proper tool for cross-cultural interpretation.
|
Medical anthropology and the illness¢disease distinction
|
|
In the English language, the terms illness and disease are synonymous and often difficult to distinguish from sickness. However, in both medical and medical anthropological circles a distinction is often made: physicians treat (and cure) diseases and patients experience (and are healed from) illnesses. Within the biomedical paradigm[1] a conceptual distinction emerged between symptoms and signs. Symptoms are ‘subjective feelings reported by the patient’ whilst signs are ‘objective indications of disease detectable by the physician’ (Evans 2003:31). This is clearly illustrated by Howard Spiro from the Yale Medical School who remarks:
As a biomedical physician, I like to discriminate between the disease, which is what the physician or the imaging technologies can detect, and the illness, what the patient feels. For me, as a gastroenterologist, disease is the stomach ulcer; dyspepsia, its pain, is the illness. (in Harrington 1997:211; see also Helman 1981:551) However, for at least two related reasons the application of this distinction to cross-cultural settings is problematic.
The fluidity of terms
The first reason is that the definition of both terms illness and disease is rather fluid. This can be illustrated by looking at the term disease which is complex and imprecise in many respects. For one, it is not always easy to identify something as a disease. Spiro remarks that the distinction between disease and illness is rather ‘fuzzy’ (1997:45) and illustrates it by asking whether hypertension is a disease or an illness. What about cancer and high cholesterol (see 1997:46)? In chronic disorders such as diabetes, ischemic heart disease or asthma it is difficult to distinguish the disease form the illness (see Kleinman 1980:74). Furthermore, it is widely acknowledged that sickness can occur in the absence of disease (see, e.g. Kleinman 1980:74) whilst someone can have a disease (such as, asymptomatic hypertension or HIV infection) without being sick (see Eisenberg 1977:11; Helman 1981:551). The view of disease as merely physical, biological or related to viruses, bacteria and the like does not even hold
up within the biomedical paradigm. In fact, within the biomedical circles of the World Health Organization (WHO) the
term disease is today used for a broad spectrum of sicknesses, the majority of which is probably sociogenic (see, e.g.
Winkelman 2009:39).[2] Even within the world of biomedicine few would think of disease as purely organic or biological. Disease, the medical anthropologist Merril Singer remarks, ‘must be understood as being as much a social as a biological product’ (1990:182). Hence, it should be kept in mind that the term disease is nowadays used (in a narrow sense)
to describe sicknesses that have organic or physical causes or to describe
(in a wider sense) any organic and physical manifestation of sickness
(immaterial whether the cause is infectious or social). It should be noted
that Murdock uses the term illness synonymous with this broad definition of disease as ‘any
impairment of health serious enough to arouse concern, whether it be due to communicable disease, psychosomatic
disturbance, organic failure, aggressive assault, or alleged accident or supernatural interference’
(1980:6).[3] In this definition the term, illness equals that of disease as covering
the whole spectrum of sicknesses. It should by now be apparent that both terms have more than one meaning
(definition) which defies the notion of an illness–disease distinction.
But there is a second reason that demonstrates this even more forcefully.
What medical anthropologists do, why they do it and how they do it
The second reason why the application of the illness–disease distinction to cross-cultural settings is
not obvious is to be found in what medical anthropologists do, why they do it and how they do it. Therefore,
as background to an understanding of the illness–disease distinction, three observations about medical a
nthropology will briefly be presented.
Medical anthropology exists by virtue of biomedicine
Medical anthropologists are anthropologists who since the end of World War II work primarily in the field of
medicine and health care. Therefore, Singer notes that the ‘job description’ of medical anthropology,
is ‘a service sector for biomedicine’ (1990:179; see also Inhorn 2010:268). Most medical anthropologists
are socialised in biomedicine and struggle with cross-cultural interpretation because of the differences between
biomedicine and the variety of health care systems they encounter. Lock and Scheper-Hughes (1990:49) point out that
one of the biggest challenges for medical anthropology is ‘to come to terms with biomedicine’.
The paradox is that the cross-cultural gap exists precisely because of the dominance (and contribution) of
biomedicine, and the challenge is not whether biomedicine will be included in a cross-cultural interpretive process
but how to account for it. Or, as Rhodes says: ‘Western biomedicine and medical anthropology are intimately connected.
Many medical anthropologists work in biomedical settings or study problems that have been defined in biomedical terms’
(1990:159).[4] Although it was not until the 1960s that the term medical anthropology was used and appreciated in
anthropological circles (see Foster 1978:3), its roots go back to interest in physical anthropology,[5]
ethnomedicine, culture and personality studies[6] and international public health.[7] The only
branch that actually concerns itself with the understanding of non-Western medical systems is ethnomedicine. The
antecedents of ethnomedicine are to be found in the work of the pioneer anthropologists who looked at all aspects of traditional
life, including sickness and health care. When examining the fruits of medical anthropology, one way is to distinguish between
theoretical,[8] clinically applied medical anthropology and critical medical anthropology. Much research in medical anthropology is conducted in conjunction with medical and health care personnel and fits into international public health programmes (see Foster 1978:8–9; Rhodes 1990:159). Critical medical anthropology, however, understands health issues ‘in light of the larger political and economic forces that pattern interpersonal relationships, shape social behavior, generate social meanings, and condition collective experience’ (Singer 1990:181; see Rhodes 1990:159). Critical medical anthropology has contributed to insights about the causes of and conditions for sickness that go far beyond the reductionistic view of the ‘germ theory’ found in the biomedical paradigm. The important point to note is that medical anthropology exists by virtue of the biomedical paradigm and is not a way of bypassing it.
 |
FIGURE 1: Two visions in medical anthropology.
|
|
Medical anthropology is no safeguard against ethnocentrism
Given their proximity to biomedicine, and, like all other anthropologists their involvement in cross-cultural
interpretation, medical anthropologists are not immune to the infections from ethnocentrism.[9] In fact,
medical anthropology as such is no safeguard against ethnocentrism, since, as the medical anthropologist Robert Hahn
points out, the socialisation of anthropologists in biomedicine ‘has led to two visions within the field of
medical anthropology as a whole, sometimes to double vision within single practitioners’ (1995:3).[10] The first ethnocentric vision, called medicocentrism,[11] follows when the superiority or universality of biomedicine is taken for granted in cross-cultural interpretation and results in alien sickness and healing episodes being dressed up in biomedical garments. As Foster (1976:773) himself a medical anthropologist complains, more often than not it happens that ‘anthropologists filter the data of all exotic systems through the lens of belief and practice of the people they know best’; and if that system is biomedicine the result is medicocentrism (for a detailed discussion of this, see Rhodes 1990). The second ethnocentric vision in medical anthropology is called xenocentrism: In the second vision, common in analyses of non-Western medical systems, researchers have professed to reveal the local
medical ‘reality’ in its own terms; in their concern not to impose their own vision on those they study,
these researchers have assumed that the local, indigenous explanations of the world of sickness and healing are valid.
[The xenocentric vision assumes] that the cultures of others have exclusive access to the truth –
at least in their home setting. (Hahn 1995:3)
By repeating the concepts, assumptions or descriptions of an alien health care system in a biomedical context is not to avoid
ethnocentrism[12] but to avoid cross-cultural interpretation. In other words, in cross-cultural interpretation ethnocentrism is avoided neither by imposing the biomedical paradigm (e.g. DSM-IV) nor by adopting the native’s point of view or the local explanation of phenomena (e.g. a so-called culture-bound syndrome). In both instances a linear comparison between health care systems results in the truth of one system being imposed onto another – xenocentrism is just the flip side of medicocentrism but equally ethnocentric (see Figure 1 for a schematic representation). The (ethnocentric) shortcoming of both visions can be illustrated by means of the two sides of the same coin (Figure 1).
On the one side is the question whether or not concepts from the DSM-IV or the ICD-10[13] can be used across cultural
boundaries.[14] On the other side is the question whether there really are conditions
(so-called culture-bound syndromes) that are incomparable to those in other cultures. Whilst the very term culture-bound syndrome[15] presupposes that some sicknesses
are culture-free or culture-blind, it can always be asked whether a certain condition in one culture is not similar to that
in another. Secondly, as insights from the multifaceted position of sickness show, humans are not only constrained by culture
but also by biology, mind, society and environment. Thirdly, the comparative view shows that local explanations neither
exhaust phenomena nor describe them exclusively. The truth of the matter is that cross-cultural interpretation cannot
take place without shared concepts. If we are trapped in our frameworks research across cultures is
impossible.[16]
Analytical models for cross-cultural interpretation can pretend to be ethnocentric-free
The third and last observation is that only analytical models for cross-cultural interpretation
can pretend to be ethnocentric-free. The hallmark of a scientific or analytical model,
Engel (1980:543) points out, ‘is that it provides a framework within which the scientific
method may be applied’ for analysis and comparison. In order to be used for analytical and
comparative interpretation of phenomena across cultural boundaries, the scientific method needs a
theoretical place to stand: ‘Observation and understanding are built from categories, hypotheses,
and principles of knowledge ... one could not begin the reconstruction of knowledge without a conceptual
platform’ (Hahn 1995:3).[17] Or, in the warning of Berry: ‘Without some established framework for making cross-cultural comparisons, I can only foresee an accumulating hodge-podge of unrelated anecdotal studies’ (1969:127). The structure of an analytical model can be illustrated by means of the African cooking-pot model.
The analogy of the three legs of the African cooking pot suggests that between the emic logic of the
culture itself and the etic logic of the dominant Western biomedical paradigm there is ‘the actual
incidence, qualitative and quantitative, of disease’ (Worsley 1982:328). And the body of scientific
knowledge about sickness and healing is much more extensive than that contained by any particular ethnomedical
model or health care system, biomedical or otherwise. Instead of a comparison (or clash) between two opposing
health care systems (the biomedical and a local paradigm) the interpretive problem can be presented as a
three-way process in which the analytical model of the interpreter serves as fixed point of comparison.
This suggestion is based on at least two theoretical principles. The first is that analytical models are different from operational folk or local health care models.
A scientific or analytical model itself is not a health care system (it does not operate as a local
health care system within a particular culture). Therefore, an analytical model is not the basis of
any dogma, medical or otherwise, and consequently, there is a huge difference between practitioners
of any health care system and cross-cultural interpreters trying to make sense of a variety of health
care systems. Unlike actual health care models, scientific models are modified and discarded if they are no longer useful. Secondly, a model of reality is not reality itself and this is particularly true of local health care systems.
Consequently, as suggested by Hahn (see 1984:14, 18, 19), a distinction should be made between a model and what
it models, an account of phenomena and what is accounted for. Health care systems, be it the biomedical or any
other health care system, are partial models of the human experience of sickness and not the totality of sickness.
Although all health care models are rational (and the biomedical model is based on science), none is in itself
an analytical or scientific tool. Despite the worldwide dominance of biomedicine since the previous century
(see Hahn 1995:131), the biomedical model remains a culture specific folk model of sickness and healing
(see Fabrega 1975; Hahn 1995:15) and is in itself not a scientific model. Whilst all health care systems
with various degrees of success highlight particular features of sickness, none captures it in totality.
The body of knowledge about sickness is far more extensive than that of any one system’s presentation.
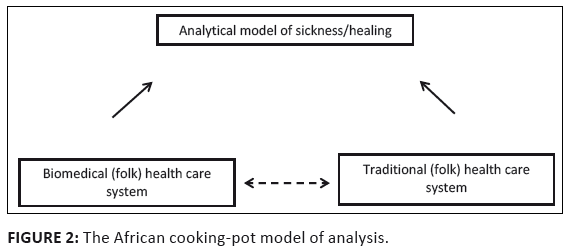 |
FIGURE 2: The African cooking-pot model of analysis.
|
|
Intercultural models for cross-cultural interpretation
Scholars concerned with ethnocentrism (medicocentrism or xenocentrism) in either biomedicine or medical
anthropology are promoting intercultural models (the third leg of the tripod) for the cross-cultural
interpretation of sickness and healing. Such models contain ideal typical descriptions of sickness and
healing that are multifaceted because they refer to the body, mind, society and environment as contributing
factors in sickness and healing. The hallmark of such models is that they do not go back beyond the 19th
century germ theory of disease but are not trapped there because all of them see health and illness
as ‘interlocking processes that are determined by biological and environmental, as well as psychological
factors’ (Fabrega 1971:389). DSM-IV and ICD-10 categories are not excluded but used together with other
conceptual tools in describing particular sickness conditions. In simple terms, an intercultural model of
sickness and healing acknowledges the wide spectrum of sickness aetiologies whilst realising that the
experience of sickness is multifaceted. Intercultural models view all sickness and healing phenomena as complex bio, psycho, social and
environmental interactions. When used for cross-cultural interpretation such models begin, though not
necessarily end, with the indigenous and personal understanding of patients (whether they are from a
traditional or biomedical framework), and when interpreting a particular sickness or syndrome, the local
understanding or experience of it is seen as necessary but not sufficient for its full description
(see Hahn 1995:54–55).[18] The primary insight of one such model, known as the
biopsychosocial model (see Engel 1977, 1980) is the multifaceted aetiology of most sickness c
onditions and the insight that effective healing consists of an integrative biopsychosocial intervention
or process.[19] The implication of such a cross-cultural model is that all sicknesses, today or in the past, whether
acknowledged by the culture or local health care system or not, are multifaceted entities. This interpretive
framework suggests that the comparison of health care systems can take place via an engagement with what is
modelled by each system whilst avoiding the ethnocentrism of imposing any one health care system onto the others.
Put differently, the local understanding and description of each and every instance of sickness and healing is
compared to the multifaceted model of sickness and healing provided by the analytical model. Comparing the biomedical health care system (paradigm) to such a framework will show that most sickness
conditions are medicalised with the search for a technical solution to all problems[20] whilst the actual instance of sickness is multifaceted. Similarly, a comparison of some traditional health care systems will show their failure to recognise organic, physiological or material factors in sickness and the need for medical intervention in many instances of sickness.
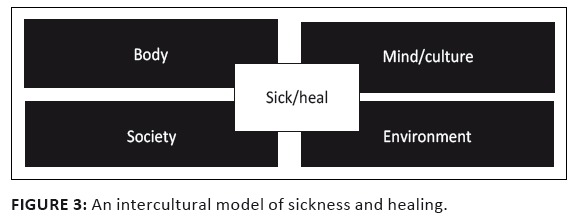 |
FIGURE 3: An intercultural model of sickness and healing.
|
|
Medical anthropology and the ambiguity of the illness¢disease distinction
If it is true that medical anthropologists have different visions on cross-cultural
interpretation, one should not expect a unified view on the illness–disease distinction.
Before looking at the different definitions of illness, it is necessary to re-emphasise that this
distinction is an affirmation of and not a transcending of the biomedical paradigm. Fully aware of
its roots in the Western biomedical paradigm, the biomedical distinction between sign and symptom is
echoed in the description of medical anthropologists Kleinman, Eisenberg and Good (1978) when they say
that the illness–disease distinction:holds that disease in the Western medical paradigm is malfunctioning or
maladaptation of biologic and psychophysiological processes in the individual; whereas
illness represents personal, interpersonal, and cultural reactions to disease and discomfort. (Kleinman, Eisenberg & Good 1978:252 [Author’s emphasis]) This is an adoption of Eisenberg definition: ‘patients suffer “illnesses”;
physicians diagnose and treat “disease”’ (1977:11). If anything, this is an
affirmation that the distinction is a product of the biomedical paradigm and not a tool to
facilitate cross-cultural interpretation between biomedical and other health care systems –
a point to be confirmed by the following analysis. The analysis will furthermore show that the
illness–disease distinction in medical anthropology is much more complex and problematic than assumed by this definition.
Illness as the response or cultural reaction to disease
The often quoted distinction by Kleinman (1980) echoes the aforementioned definition of illness as dependent on disease: Disease refers to a malfunctioning of biological and/or psychological processes,
while the term illness refers to the psychological experience and meaning of perceived disease.
Illness includes secondary personal and social responses to a primary malfunctioning (disease) in the
individual’s physiological or psychological status. (Kleinman 1980:72) In this formulation the illness–disease distinction is not only a replication of the
symptom–sign distinction in biomedicine but also displays the medicocentric vision of
biomedicine. According to this understanding, illness is dependent on disease since illness
is defined in terms of disease;[21]the two express different interpretations ‘of
a single clinical reality’. In this definition, Kleinman insists, illness and disease are
not entities but ‘explanatory concepts’ (1980:73). Schematically it can be presented in Figure 4. Within this understanding disease is universalised (when people are sick they suffer from some
kind of a disease) whilst patients’ experiences (their reactions) are localised as illnesses.
Illness as an independent entity from disease
In what can be called the independent definition, the understanding of illness is not dependent on disease.
To once more quote Kleinman, Eisenberg and Good (1978): physicians diagnose and treat disease (abnormalities in the structure and function
of body organs and systems) whereas patients suffer illnesses (experiences of disvalued
changes in states of being and in social function; the human experience of sickness).[22] (Kleinman, Eisenberg & Good 1978:251) About this definition Eisenberg says (1977:11): ‘Illness and disease, so defined, do not stand
in a one-to-one relationship’. In other words, illness is not dependent on disease.[23]
In this understanding there are illnesses that exist independently from disease and are no response to
any disease.[24] Schematically it can be presented in Figure 5. In an attempt to give expression to Kleinman’s application of the double vision, the medical
anthropologist Allan Young suggests a schema where there are illnesses without disease counterparts
and vice versa (see 1982:266). Schematically this position can be presented in Figure 6. But you cannot have your cake and eat it! Illness cannot both be a response to disease and
represent independent entities. Whilst realising this dilemma, Young altered the definition of
illness to ‘a person’s perceptions and experiences of certain socially disvalued states,
but not limited to, disease’ (1982:265). However, the term illness cannot be used both for the response to disease
and for independent sicknesses (or disvalued states) next to disease. And the attempt to avoid
some of these problems by insisting that neither illness nor disease are entities, but concepts
(see Fabrega 1971:390; Kleinman et al. 1978:252; Pfifferling 1981:210) is unsuccessful
because once it is admitted that disease is not a thing – only a concept –
there is no thing of which illness can merely be the subjective cultural experience (see Eisenberg 1977:18).
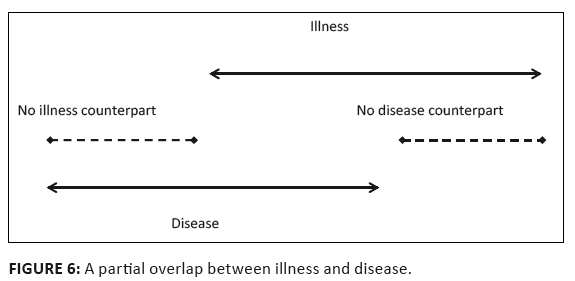 |
FIGURE 6: A partial overlap between illness and disease.
|
|
Illness as a label for traditional health care systems
It is a small step from the notion of illness as entity independent
from disease to the idea that the sicknesses experienced and described by traditional health
care systems are merely illnesses. When the terms illness and disease are used to
describe entire health care systems, the nature–culture dichotomy often kicks in, in order
to label traditional health care systems as merely concerned with illness whilst it is maintained
that traditional healers can only heal illnesses. The root of this notion is visible in the following description:Medical anthropologic studies show that traditional healing in developing societies
and popular health care in our own are principally concerned with illness, that is, with
treating the human experience of sickness. Healers seek to provide a meaningful explanation
for illness and to respond to the personal, family, and community issues surrounding illness. (Kleinman et al. 1978:252)[25] Even if it were the case that people in traditional societies experience sickness similar to
popular conceptions of patients in Western societies (and one can understand the comparison),
it does not mean that they are not suffering from potential diseases. The fallacy of this dichotomy
between, on the one hand, the biomedical and, on the other hand, popular notions of sickness in Western
societies and local understandings in traditional societies, is to equate the local description (or experience)
with the totality of the sickness. Even if a sickness is experienced as an illness, this does not mean someone
is not suffering from an identifiable disease. Besides the fact that this distinction presupposes the biomedical paradigm[26]
(see Hahn 1984:19 in this regard), it reverts back to the dichotomous notion of sickness
as either physical (real) or mental (not real) whereas the best theories today take into account the multifaceted nature
(physical, individual, social, etc.) of sickness. In many instances, and this is one of them, the illness–disease distinction
is a variant of the mind-body and the culture-nature dichotomies (see Lock et al. 1990:53; Rhodes 1990:166).
As illustrated earlier, this easily happens in the case of so-called culture-bound syndromes where an outdated
definition of disease as bodily (natural) entity informs such dichotomies.
Illness as the effect or impact of disease
In yet another formulation the definition of illness is extended to include the effect of sickness symptoms on
patients. Medical anthropology, Kleinman (1986b) says:has advanced a technical distinction between ‘illness’ and ‘disease’ with illness
defined as socially learned and culturally shared ways of perceiving, labelling, experiencing, and reacting to symptoms.
This includes most notably the personal and interpersonal problems illness creates or intensifies. (Kleinman 1986b:230 [Author’s emphasis]) This definition of illness covers the personal and cultural response as well as the labelling of diseases,
but, it also includes the personal and social impact of sickness. Schematically this position can be presented in Figure 7. This understanding of the illness–disease distinction is no tool for cross-cultural differentiation
because irrespective of the kind of disease someone suffers from, within all cultural settings people will
experience some effect or impact of sickness. And needless to say that illness thus defined has no cross-cultural
currency – it merely is a label for the individual impact or effect of disease, whether infectious or
non-communicable. Even though the impact will be mediated by or be dependent on culture it does not in any way
facilitate cross-cultural interpretation.
 |
FIGURE 8: Illness, disease and disorder as different expressions of suffering.
|
|
Illness as the patientÆs understanding of sickness
For the sake of being comprehensive it should be noted that Hahn – who rejects both ethnocentric
(linear) visions of anthropology but sees cross-cultural interpretation in terms of the tripod analytical
model – suggests that together with disorder, the terms illness and disease can be used to refer to
different ideologies (perspectives) of sickness. He suggests that the same suffering or sickness experience
can be viewed from any of three ideological positions but primacy is given to illness ideology.
The illness perspective is the patient’s understanding of suffering and should be given priority
in any diagnosis, be it as the starting point for comprehending the sickness only. When the same suffering
episode is described from the perspective of biomedicine, he calls it a disease ideology whilst the perspective
from varied traditional healers (non-Western health care system) is referred to as a disorder ideology (see 1984:15–16). Because biomedicine is ‘the dominant folk model of disease in the Western world’ (Engel 1977:130),
the illness experience of Western people will tend to simulate the disease ideology whereas the suffering of people
from other health care systems (their illness) will simulate their own folk understanding. Therefore, any suffering
(or disease in the broad sense of communicable or non-communicable diseases) can be experienced as different illnesses
depending on the person’s local health care system. Schematically this position can be presented in Figure 8. The logic of this proposal can be illustrated by means of HIV and AIDS. For Western people the sickness
or suffering will be experienced as an infectious disease whilst for most African people today it is
experienced as an illness resulting from witchcraft (see Ashforth & Nattrass 2005:289; Dickinson 2008:283).
Neither of these affirms or denies anything about the impact or effect of the illness on the individual or his
or her community but departs from the dominant aetiology explanation of different local health care systems.
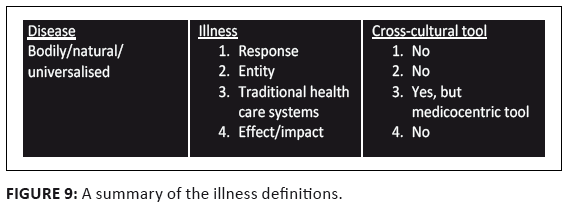 |
FIGURE 9: A summary of the illness definitions.
|
|
Summary remarks on the illness¢disease distinction in medical anthropology
The illness–disease distinction in medical anthropology indeed contributes to sensitise biomedical
practitioners as well as social scientists to the multifaceted aetiology of sickness and the complex nature
of sickness experiences (see Lock et al. 1990:53). It provides the basis for studying the influence of
cultural factors (beliefs, issues of meaning and cultural experiences) and context (social, economical and political
conditions) on the construction and experience of sickness (see Rhodes 1990:165). However, it is not unproblematic in
medical anthropological circles. First of all, there is not a or the definition of illness and disease and the semantic status of both
terms is by no means unequivocal and in many respects the source of confusion because of covert forms of ethnocentrism.
The paradox is that in some instances the notion of disease is relativised to the Western medical paradigm with illness
belonging to ‘the other’ and in other cases disease is universalised and given primacy – something to
which illness is only a secondary and culturally variable reaction (see Hahn 1984:10). The preceding analysis supports
the finding of Hahn (1984:1), who after reviewing some of the major works on the illness–disease distinction in
medical anthropology, concludes that this distinction ‘has been made inconsistently from work to work, and even
within works’ – and these differences largely correlate with the different anthropological visions. Secondly, medical anthropology as such is not a tool for cross-cultural interpretation and does not automatically
protect from ethnocentrism. On the contrary, by design it often invokes either medicocentrism or xenocentrism.
Much of medical anthropology itself suffers from medicocentrism and/or xenocentrism because of the linear
comparison of health care systems – the question is which health care system is privileged in the comparison.
To say it once more, medical anthropology as such is no safeguard against ethnocentrism but the site of its struggle
and the above discussion bears that out. Consequently, the illness–disease distinction is not simply a tool for
cross-cultural interpretation but was designed within the clinical setting dominated by the biomedical paradigm in
order to account for the cultural gap. Disease and illness are terms that describe the same sickness phenomenon
from different perspectives and neither is a tool to distinguish different kinds of sicknesses nor a way of
discriminating between various health care systems. The illness–disease distinction does not avoid the
biomedical paradigm but in practice assumes biomedicine. Thirdly, whilst little has been said about the medicocentric definition of disease that is assumed in this
distinction, it remains remarkable that of the four definitions of illness and disease, only one pair functions as
a cross-cultural tool. Neither as response to disease nor as independent entity nor seen as the impact of sickness can illness be taken as a
tool to understand ethnomedical descriptions of sickness in a biomedical world. Ironically, it is only in the third
definition where illness is used to label traditional health care systems that it functions in a medicocentric way as a
tool for cross-cultural interpretation.[27] The ethnocentric labelling of
all traditional health care systems
as merely concerned with illness is hardly an improvement on traditional medicocentrism. Once the biomedical definition of disease is eroded from its ethnocentric position, it becomes apparent
that all sicknesses are biopsychosocial phenomena, some with and others without identifiable infectious disease
aetiologies. Whatever the actual aetiology of a sickness, it can be individually, socially and culturally experienced
in unique ways. In view of these considerations, universalising the disease model is not only ethnocentric
(a case of medicocentrism) but irresponsible, because no justice is done to the complexity of human sickness conditions. Fourthly, when no clear distinction is made between reality and models of reality, accounts
of phenomena are identified (or confused) with the phenomena accounted for. This happens when sickness
constructions of health care systems are taken as the sickness. When applying the scientific vision,
such as the biopsychosocial model of sickness, it is much easier to see that each local health care model
provides an understanding of complex biopsychosocial phenomena, albeit some in very reductionist ways.
This point can be illustrated by means of the HIV and AIDS pandemic. A large percentage of people in
southern Africa infected with the HI-virus claim that they are ‘bewitched’ or are sick because of the Devil.
The belief of bewitchment does not mean they are not HIV positive. What it does say is that the same sickness condition
can be described by means of various explanatory models, but how to cross the cultural gap between them is another matter.
|
The illness¢disease distinction in New Testament scholarship
|
|
Within the social-scientific project it is undoubtedly rhetorically powerful to claim that the
illness–disease distinction is a ‘basic distinction’ in medical anthropology
(or as Crossan does, in echoing the words of Kleinman, to call it a ‘key axiom’
in medical anthropology). In addition to the fact that there is no such fundamental distinction
and that it functions within particular anthropological visions only, an analysis of the illness–disease
distinction in New Testament scholarship will reveal a rather disconcerting picture. It appears that New Testament
scholars seem oblivious to the fact that the terms illness and disease are used in medical anthropology
with a variety of meanings, and that the distinction is not a tool for cross-cultural interpretation. Consequently,
they invent a different spectrum of meanings for the terms and instead of avoiding medicocentrism this distinction
functions to promote ethnocentric understandings of Jesus’ healings within disguised theological or ideological agendas.
These are strong claims that need to be substantiated.
The variety of definitions of illness and disease in New Testament scholarship
From reading New Testament scholarship on the illness–disease distinction one will not know that there is no a or the definition of the terms in medical anthropology. In fact, New Testament scholars are either oblivious of the fact that the terms have a variety of meanings in medical anthropology and the biomedical paradigm or they deliberately conceal them in service of another agenda. This is apparent from the way the distinction is presented. When Eve calls on Kleinman’s ‘careful distinction’[28] in order to
present illness as the impact or effect of sickness, it is done at the expense of all the other definitions that Kleinman also
promotes.[29] This represents not only a limited understanding of the terms but a deliberate exclusion of those
definitions that would undermine his argument. But it is in the mixing of meanings under the pretension that there is a or the single set
of definitions of the terms illness and disease that the distortion can best be seen. Although
it starts with Pilch, it is in the work of John Dominic Crossan who follows Pilch religiously[30]
that the creative (distorted) exegesis of these terms can be illustrated. In his book on the historical Jesus, Crossan ascribes the illness–disease distinction to George Peter Murdock
(see Crossan 1991:319) and then claims that Arthur Kleinman distinguishes ‘as Murdock above’ between
illness and disease with illness seen as the psychosocial and cultural response to disease (see 1991:336).
Three years later Leon Eisenberg and Kleinman are presented as the champions of medical anthropology ‘or
comparative ethnomedicine’ [author’s emphasis] who in Crossan’s (1994:80) words
propose ‘a basic distinction’ between illness and disease. However, Crossan starts with the dependent
definition of illness (as a response to disease) but with a sleight of hand combines it with the medicocentric view
which sees all traditional health care systems as merely concerned with illness. For this we have to return to the
tradition history of the terms as employed by him, starting with Murdock and following his presentation to
Eisenberg and Kleinman. It is simply a misrepresentation of Murdock to link his name to this illness–disease distinction because, as
shown earlier, he uses the term illness synonymous with sickness as referring to all kinds of diseases. However,
Crossan’s use of Eisenberg and Kleinman is even more disconcerting. The definition of Eisenberg used by
Crossan is the independent one and in Eisenberg’s article is followed by the following words: ‘Illness
and disease, so defined, do not stand in a one-to-one relationship’ (1977:11) – in other words, it is
not merely a response to disease. Crossan not only omits these words, but without any reference to the latter
pages replaces them in the same quotation with words from a paragraph three pages down (in a different argument)
that suggests that indigenous healers can only treat illnesses. Illness is thus presented as if Eisenberg
suggests that it is a legitimate (medicocentric) label for traditional health care systems. On the very page
Crossan’s second authority for the illness–disease distinction is Kleinman’s dependent definition
of illness as the response to disease (see Crossan 1994:81). By combining Murdock’s definition of illness as umbrella term for all sicknesses with Eisenberg definition of
illness as an independent entity together with Kleinman’s notion of illness as merely a response to disease,
Crossan comes up with a mixed bag that assigns the features of the dependent definition to the others. Therefore, in his
view, ‘the leper who met Jesus had both a disease (say, psoriasis) and an illness, the personal
and social stigma of uncleanness, isolation, and rejection’ (1994:82). Furthermore, the features of the
dependent definition that people always assign meaning to sickness (construct illnesses) are then transferred to
traditional health care systems with the claim that folk healers always successfully heal illnesses. Jumping between definitions, however, started with Pilch (as will be illustrated at a later stage). Here the focus
is on the claim promoted by him that healing always takes place but that curing is rare. Besides the fact that features
of one meaning of illness are transferred to the other, common sense tells us that neither one of these claims is true.
If curing was rare, most people alive today would be sick because most of us have at some point suffered from an infectious
disease (such as the common flu). But the truth is that many (if not most) infectious and congenital diseases are today very
effectively cured by medical treatment.[31] It is the sociogenic diseases that are hard to
deal with and, like today,
many people in Jesus’ day must have suffered bodily sicknesses that were not caused by germs.The fact that people
always assign meaning to sickness (assign symptoms to their sickness signs) does not mean healing automatically takes place. Furthermore, the notion that people always find meaning in sickness (which, might or might not be the case in reality)
cannot support either of the historical claims that Jesus probably healed (or potentially could heal) what is called mere
responses to diseases (illness). And even if patients always and infallibly experience meaning in sickness, it does not
follow that healers automatically have an effect on sicknesses that are not caused by viruses, bacteria and the like (whether
they are called culture-bound syndromes or sociogenic diseases and psychogenic diseases). Local explanations cannot remove or
replace the sickness reality caused by infectious diseases. Perhaps more remarkable (and disturbing) is the fact that no New Testament scholar after Pilch and Crossan whilst
quoting the very same sources, has either picked these discrepancies up or even noted the variety of definitions
within medical anthropology. It should be of great concern for the social-scientific project in New Testament
interpretation if social science and anthropological material is used in such an uncritical and proof texting way.
Raiding these disciplines for ‘insights’ (like fundamentalists raid biblical texts for proof) cannot advance responsible
interdisciplinary research. But there is more to the confusion of these ‘insights’ in New Testament scholarship, because
not only are these studies used in an uncritical way, they are used so in different ways. It should be noted that whilst citing the
same medical anthropologists (often even the same words) New Testament scholars come up with distinct definitions of their own
for illness and disease.
Illness and disease as tools for cross-cultural interpretation?
The primary function of the illness–disease distinction in New Testament scholarship is to serve as a tool for
cross-cultural interpretation of Jesus’ healing stories. But it is precisely in these attempts that the new
ethnocentrism is revealed and theological or ideological agendas are promoted. I will start with the viewpoint of Crossan. Crossan’s position is captured in the often repeated example of the film Philadelphia (1993) where the main character is
suffering from HIV and AIDS, and whilst the disease could not be cured, his illness was healed (see 1994:81, 1998:294, 2009:128).
Applied to the blind, the lame or the deaf encountered in the gospel stories, Crossan maintains that they were suffering from some
kind of common disease that Jesus could do nothing about whereas their illnesses
he could heal.[32] By this Crossan is providing a powerful historical explanation as to what the historical Jesus was doing during the
so-called healing miracles. At least for the healing stories that he considers authentic, people were suffering
from specific diseases (sickness conditions which can be attributed to specific biological or organic defects and can
only be treated by medical practitioners) that Jesus could not cure and therefore, he only offered therapeutic
comfort – he ‘healed’ them, seeing that illness as the response to disease can easily and effectively
be healed by a folk healer. In his words: ‘for disease you are better off with the doctor and the dispensary, but
for illness you are better off with the shaman and the shrine’ (1991:336).[33] Here the nested assumption is that the patients were suffering from diseases that were experienced as illnesses and the latter can effectively be healed by a folk healer. This assumption derives from the mixing of definitions (as shown earlier). Whilst Pilch apparently also promotes this position, analysis shows that his tool kit contains a different set of meanings. It is not without reason that I started with Crossan, because it is much more difficult to make sense of Pilch’s
arguments.[34] He departs from the definition of illness and disease as formulated by Kleinman[36] (see Pilch 2000a:13, 25, 59–60, 93, 2008:98) and, similar to Crossan, illustrates it with a contemporary (and very personal) example of a patient (his late wife) suffering from ovarian cancer. Although she was not cured, despite the best available chemotherapy she was 100% healed because healing, the restoration of meaning to life, Pilch says ‘occurs always’ (2000a:141). According
to this understanding Jesus did not and could not cure any disease but only healed some illnesses.[36]
This is based on Pilch’s belief that ‘cure is a relatively rare occurrence in human experience’ (2000a:141) and in his
specific understanding of the distinction between curing and healing, ‘curing is efficacious when biomedical changes take place;
healing is efficacious when the people who seek it say it is’ (2000a:34). Therefore, the kind of healing that Jesus was involved
in, was symbolic healing in which the healer mediates culture, and when, for instance demons were exorcised, the anxious client believed
the cause of the problem was gone. What took place was a transformation of the experience of the patient (see 2000a:32, 35).
What Jesus did was to reintegrate people into society: ‘He restored meaning to the lives of these collectivistic persons’
(2000a:142).[37] It is clear that in this understanding, depending on the perspective, the same human condition is either a disease
(the real bodily or material defect) or an illness (the mindful experience). Again, an insight with far-reaching implications:
New Testament documents were not concerned with disease but with illness, which reflects a sociocultural perspective and
healing involves the provision of personal and social meaning and therefore ‘all illnesses are
always and infallibly healed’ without the disease necessarily affected (2000a:93; and see Pilch 1991:190–192).
All of this presupposes the dependent definition of illness. It might seem as if Pilch is saying the same thing as Crossan but his position is a little more confusing,
as illustrated by the example of moonstruck, the term used by Matthew (17:15 and see 4:24) to describe
the condition of a boy from whom Jesus exorcised a demon. Pilch claims that it is ‘irresponsible and grossly unfair’
(2010:153) to translate and understand it as an instance of epilepsy. This is not surprising for he says: ‘Given the absence
of scientific terminology in antiquity, it seems best to speak of illnesses rather than diseases in the Bible’ (Pilch 2008:98).
Moonstruck was an illness that should not be treated as if it were a disease in order to make it accessible to modern interpreters;
moonstruck cannot be considered epilepsy but is an instance of a ‘culture-bound syndrome’ (Pilch 2000a:19).
Here a sudden but significant change of definition occurs, as illness no longer is the response to a disease because if it were,
it could well have been the cultural response to, say, epilepsy. But Pilch uses a different definition of illness and disease to
argue the opposite, namely, that moonstruck was definitely not epilepsy and he gives it another twist by saying that it
(the illness) should be seen as a culture-bound syndrome. This is also the case with leprosy
mentioned in the Gospels which most certainly were not instances of Hansen’s disease but should according
to Pilch also be considered culture-bound syndromes (see Pilch 2000a:54). Whatever the precise conditions, Pilch
claims that they were not ‘diseases’ but ‘illnesses’ (see 2000b:131). After ruling out Hansen’s
disease (because no evidence for its existence in 1st century Palestine has been confirmed) it is postulated that
these ‘marks’ on the skin of the patients were only illnesses. The reasons being that without biomedical
knowledge and microscopes the ancients would not have been able to identify ‘diseases’ whilst their cultural
interpretation of the conditions suggests these were mere illnesses (see Pilch 2000b:131).[38]
Similarly, it is medicocentric to consider the eye condition mentioned in Matthew 9:27–31 as the healing of a cataract
(see 2008:101) whilst conditions resulting from the evil eye are also culture-bound syndromes or folk-conceptualised
disorders (2000a:19). Unlike Crossan who claims that these illnesses were responses to diseases, Pilch clearly operates in the
preceding arguments with illnesses as independent entities from disease. Remarkably, both claim the features
of the independent definition of illness (that illnesses are always healed). In addition, they share the linear
structure of cross-cultural interpretation but within different anthropological visions.
The impact of a linear interpretive process
Whilst both Pilch and Crossan employ the illness–disease distinction they do so in different ways:
both follow the linear logic but part ways in that one follows a xenocentric and the other the medicocentric
anthropological vision. Pilch is to be credited for insisting that the New Testament healing stories cannot
simply be framed in terms of biomedical categories but then falls into the xenocentric trap by insisting that
the interpreter should respect the emic understanding of health and sickness (moonstruck is not epilepsy and demon
possession is not multiple-personality disorder). Unfortunately, this claim merely rests on the xenocentric position
that takes the local understanding as the full one. The fallacious implication of this kind of reasoning is that if no
laboratory is around, people cannot suffer from diseases (such as epilepsy or HIV and/or AIDS). In this view, cross-cultural
interpretation takes place when biomedical categories are avoided and local explanations are endorsed. But this happens at the
expense of Pilch’s own definition of illness as a response to disease. He transfers one of the features from this
definition of illness to that of illness as an independent entity: because illness as response always takes place and
results in healing (which, by the way, is not necessarily true), it does not mean that illness as independent entity
(such as culture-bound syndromes) is always and infallibly healed. Crossan on the other hand, assumes that people were sick because they were suffering from diseases
(such as leprosy as a skin condition) that were experienced as illnesses and a folk healer such as
Jesus could only heal the illnesses and do nothing about the diseases. This is medicocentrism in its
authentic garment where the ideas of biomedicine are universalised and applied to all other cultural
settings whilst relegating traditional healers to therapists of illnesses. Claiming that 1st century Mediterranean people only experienced illnesses although diseases were around
(see Pilch 2008:98) is as reductionistic (and misleading) as saying that they were really sick but satisfied
with healing. Donald Capps (2008:xvii), in my view, is correct in saying about this view of Jesus’
healings: ‘The miracle is in the fact that the illness was healed without the disease being cured’
(and see the criticism of Avalos 1999:26). At the very least the dichotomy between healing and curing as cross-cultural
tool is a distortion and misrepresentation of medical anthropological research. If and when that distinction is made,
it is important to ask what it is made for. For example, Kleinman himself is aware of the complexity of the healing process;
cultural healing, he says, is only part of the healing process because ‘the healing process usually involves
two related activities – the provision of effective control of the disease and of personal and social meaning of the
experience of illness’ (1986a:35).[39]
But these dichotomies are precisely the result of the linear way of conducting cross-cultural interpretation.
Not only is the illness–disease distinction suffering from a random mixing of features from the different
definitions, it also remains trapped in the ethnocentric visions of cross-cultural interpretation.
The solution, in my view, is not a refinement of either of these visions but the development of an intercultural model
that operates in a different way (the African cooking-pot model).
Healing illnesses as acts of political resistance
If the preceding claims are true that New Testament scholars pay no attention to the diversity of definitions in medical anthropology and randomly pick and choose meanings or definitions, the question remains as to why this happens. To what end is the illness–disease distinction employed in New Testament scholarship? I want to suggest a theological motif that functions in opposition to traditional theological and scholarly claims that Jesus’ healings should be seen as miraculous cures. The employment of medical anthropology in general and the illness–disease distinction in particular is an attempt to avoid the medicocentrism of the position which maintains that the patients encountered by Jesus were suffering from serious diseases, and because Jesus was no medical practitioner, healing them must have resulted from miraculous deeds (see Craffert 2008:254–255 for examples of this approach). Whilst the texts’ claims that Jesus healed successfully are taken at face value, other explanations must be offered for this success and nothing is more useful than the concocted picture of illnesses. Either in the garment of culture-bound syndromes or as mere reactions to diseases, the healing of illnesses became the scapegoat to carry the successful deeds of the historical Jesus. Yes, Jesus healed, the implicit argument goes, either mere illnesses or culture-bound syndromes that can easily be treated by a folk healer. But there must be something more to these healings as, apparently, it is not enough to claim that the historical Jesus healed such conditions. Compared to a Jesus who performed miraculous deeds this is unimpressive and therefore an additional explanation is offered as to what Jesus was doing in healing illnesses. This is where modern political ideology comes into the picture: in the healings Jesus actually performed deeds of political resistance if not treason. And again, illness is the vehicle or scapegoat to carry the burden. Two examples will suffice. Since, as the texts claim, Jesus successfully healed people and because they only suffered from illnesses and not diseases, there seems to be an urge to ascribe some powerful meaning to these acts. This is what is happening in Pilch’s most recent suggestion that Jesus’ healings could be seen as ‘treasonous political behavior’ (2010:154). Based on the distinction that illnesses are not diseases,[40] they were not the
physical problem. The state of pollution or loss of meaning was, and therefore, healing only addressed and restored the
latter. For this argument Pilch relies on the work of Moerman and suggests that the ‘meaning response’ is the
process by means of which healing was mediated by Jesus (see Pilch 2010:147). The provision of meaning is based on power
and authority and Jesus acted as distributor of meaning and in that way he could be a successful healer. The problem was
that he occupied no recognised position of power or authority and that infuriated the authorities: ‘Since authorities
did not authorize this use of power, Jesus was given the death penalty for his treasonous activity’ (Pilch 2010:154). In this argument illness is no longer the assignment of meaning to disease, but Jesus is the one providing
meaning, and since meaning is the means of healing illness, Jesus’ healings of illnesses are taken as
secure facts. It is unfortunate that, based merely on the occurrence of the term meaning in the dependent
definition of illness (as the provision of meaning to disease) and in the term meaning response, that this connection is made.
The meaning response[41] (placebo effect) as the effect of any therapy on the body based on perceived meaning by a patient
has absolutely nothing to do with the experience of sickness. Put the other way round, whether sickness is experienced as
meaningful (an illness) or not and whether someone is suffering from any kind of disease experienced as an illness is
totally unrelated to the meaning response. The latter refers to the fact that therapeutic actions are perceived as
meaningful and thus impact on a patient. In fact, the meaning response is the most common denominator researchers
in biomedicine are trying to eliminate in the testing of medications. If Jesus as folk healer activated a meaning
response (therapeutic process) it has nothing to do with whether people experienced their sickness meaningfully or
not and is no indication that they only suffered from illnesses. For Horsley Jesus’ exorcisms, in particular the Beelzebul pericope, can be understood as a political act and more
precisely as a form of political resistance and symbolic defeat of Roman rule. Based on the illness–disease distinction
he suggests that illness ‘often involves particular relationships of power, domination, and deprivation’ (2008a:85).
Consequently, he treats the accounts of demon possession as mere illnesses and Jesus’ exorcisms as defeat of Roman rule
(see 2003:102–109). As illnesses (which were not diseases) he argues that these stories were told and were heard by
1st century Mediterranean audiences as (symbolic) defeats of Roman Imperial power. If the endorsement or dismissal of these accounts as miracles and magic constitute a reductionism as claimed by Horsley
(see 2008a:85), then presenting them merely as symbolic acts of political resistance is a reduction, if not misrepresentation,
of a different kind. Biopsychosocial sickness episodes are reduced to illness accounts brought on by Roman imperialism
(see 2003:109) whilst the complexity of such human experiences is neglected. There is no doubt about the relationship
between spirit possession as the congenital psychological mechanism of dissociation and sociocultural, economic or
political circumstances (see, e.g. Bourguignon 2005). But this does not mean that all instances of spirit or demon
possession can be reduced to such circumstances because as Bourguignon (see 2005:376) shows, instances of non-trance
possession are a major explanatory theory for the presence of disease in many settings. Demon possession can simply
be the local explanation for disease (such as bewitchment functions for many as explanation for HIV or AIDS) and the
illness–disease distinction as such is no justification for such a claim about the nature of the condition.
This article started with the observation that in some circles Jesus research is dramatically influenced by the
employment of medical anthropology in general and the illness–disease distinction in particular. Claims are made that medicocentrism is avoided
whilst cultural sensitive readings provide cross-cultural interpretation and understanding of the healing accounts
in the gospels. In view of the above discussion it should be asked whether any of these claims are true and whether
as a taxonomic scheme, the illness–disease distinction obscures or facilitates cross-cultural interpretation. Pilch is to be credited for creating an awareness of both the cross-cultural comparative tasks and the potential of
medical anthropology for dealing with the healing accounts in the gospels. Unfortunately, his own application as well
as that of his closest followers suffer from a selective poaching of ‘insights’ or concepts from medical
anthropology without really engaging in cross-cultural interpretation. It is difficult to escape the suspicion that the
illness–disease distinction functions in Jesus research to serve a theological or ideological agenda. Whilst it is
in many circles no longer fashionable to say that Jesus’ healings were extraordinary miracles, it is theologically
convenient to uphold their historicity by classifying them as healings of illnesses. Perhaps the biggest challenge for
New Testament scholars who want to move into interdisciplinary and cross-cultural interpretation is to move away from
simplistic and one-dimensional explanations and to come to grips with the complexity of the relationships between culture,
body and society. Ultimately, moonstruck, bewitchment and the explanation of a virus are only ethnomedical labels for
conditions that are by nature complex biopsychosocial phenomena. If it cannot be said that bewitchment excludes the
diagnosis of HIV and AIDS, does moonstruck exclude epilepsy? From this perspective it is easy to see that moonstruck
is a culture-bound explanation for something that could (or could not) have been epilepsy (an issue that cannot a priori be
settled by the illness–disease distinction). Although he is not a New Testament scholar, Capps applies biomedical insights in his cross-cultural interpretation
of Jesus’ healings in another medicocentric way but one that suggests the importance of a scientific model
for doing cross-cultural interpretation. He suggests that most of the conditions mentioned in the New Testament
could be taken as somatoform disorders as defined by the DSM-IV (see 2008:3–14). These are conditions
with physical, organic symptoms caused by psychosocial factors and are not treated as pure ‘medical’
conditions. It is an empirical question whether the category of somatoform disorder is used by him to shape or
illuminate the data.[41] The eternal predicament of anthropological psychology is characterised by the oscillation between assuming a psychic unity of humankind (universally applicable nosology) and a cultural relativism of psychological functioning (a diversity of mental disease, varying from culture to culture). Analytical models of sickness aim at mediating between these two because they treat both sickness and healing as complex configurations of biopsychosocial phenomena.
I offer this article as a tribute to Prof. Andries van Aarde who has worked relentlessly to introduce and encourage the use of the social sciences and the social-scientific perspective in South African New Testament scholarship.
Ashforth, A. & Nattrass, N., 2005, ‘Ambiguities of “culture” and the antiretroviral rollout in South Africa’, Social Dynamics 31(2), 285–303.
doi: 10.1080/02533950508628716
Avalos, H., 1999, Health care and the rise of Christianity, Hendrickson, Massachusetts, MA. Berry, J.W., 1969, ‘On cross-cultural comparability’, International Journal of Psychology 4(2), 119–128.
doi: 10.1080/00207596908247261
Bourguignon, E., 1968, ‘World distribution and patterns of possession states’, in R. Prince (ed.), Trance and possession states, pp. 3−34, Burke Memorial Society, Montreal.
doi: 10.1177/136346159202900406
Bourguignon, E., 1992, ‘The DSM-IV and cultural diversity’, Transcultural Psychiatric Research Review 29, 64–114.
doi: 10.1002/9780470996409.ch21
Bourguignon, E., 2005, ‘Spirit possession’, in C. Casey & R.B. Adgerton (eds.), A companion to Psychological Anthropology: Modernity and psychocultural change, pp. 374−388, Blackwell, Oxford.
doi:
10.1002/9780470996409.ch21
Capps, D., 2008, Jesus the village psychiatrist, Westminster John Knox, Louisville, KY/London. Craffert, P.F., 2008, The life of a Galilean shaman: Jesus of Nazareth in anthropological-historical perspective, Cascade, Eugene, OR. Crook, Z.A., 2009, ‘Review of Capps, D Jesus the village psychiatrist’, Biblical Theological Bulletin 39(1), 48–49.
doi: 10.1177/01461079090390010604
Crossan, J.D., 1991, The historical Jesus: The life of a Mediterranean Jewish peasant, Harper, San Francisco, CA. Crossan, J.D., 1994, Jesus: A revolutionary biography, Harper, San Francisco, CA. Crossan, J.D., 1998, The birth of Christianity: Discovering what happened in the years immediately after the execution of Jesus, HarperSanFrancisco, San Francisco, CA. Crossan, J.D., 2009, ‘Jesus and the challenge of collaborative eschatology’, in J.K. Beilby & P.R. Eddy (eds.), The historical Jesus: Five views, pp. 105−152, IVP Academic, Downers Grove, IL. Dawson, A., 2008, Healing, weakness and power: Perspectives on healing in the writings of Mark, Luke and Paul, Paternoster, Milton Keynes/Colorado Springs, CO/Hyderabad. Dickinson, D., 2008, ‘Traditional healers, HIV/AIDS and company programmes in South Africa’, African Journal of AIDS Research 7(3), 281–291.
doi: 10.2989/AJAR.2008.7.3.5.652
Eisenberg, L., 1977, ‘Disease and illness: Distinctions between professional and popular ideas of sickness’, Culture, Medicine and Psychiatry 1, 9–23.
doi: 10.1007/BF00114808 Engel, G.L., 1977, ‘The need for a new medical model: A challenge for biomedicine’, Science 196(4286), 129–136.
doi: 10.1126/science.847460
Engel, G.L., 1980, ‘The clinical application of the biopsychosocial model’, American Journal of Psychiatry 137(5), 535–544. Evans, D., 2003, Placebo: Mind over matter in modern medicine, HarperCollins, London. Eve, E., 2002, The Jewish context of Jesus’ miracles, Sheffield academic Press, Sheffield. Fabrega, H. (Jr.), 1971, ‘The study of medical problems in preliterate settings’, Yale Journal of Biology and Medicine 43, 385–407. Fabrega, H. (Jr.), 1975, ‘The need for an ethnomedical science’, Science 189, 969–975.
doi: 10.1126/science.1220008
Foster, G.M., 1976, ‘Disease etiologies in non-Western medical systems’, American Anthropologist 78, 773–782.
doi: 10.1525/aa.1976.78.4.02a00030
Foster, G.M., 1978, ‘The new field of medical anthropology’, in G.M. Forster & B.G. Anderson (eds.) Medical anthropology, pp. 1–10, John Wiley & Sons, New York. Frankenberg, R., 1980, ‘Medical anthropology and development: a theoretical perspective’, Social Science & Medicine 14B, 197–207. Hahn, R.A., 1984, ‘Rethinking “illness” and “disease”’, Contributions to Asian Studies 18, 1–23. Hahn, R.A., 1995, Sickness and healing: An anthropological perspective, Yale University Press, New Haven, CT/London. Harrington, A. (ed.), 1997, ‘Placebo: Conversations at the disciplinary borders’, in A. Harrington (ed.), The placebo affect: An interdisciplinary exploration, pp. 208−248, Harvard University Press, Cambridge, MA. Helman, C.G., 1981, ‘Disease versus illness in general practice’, Journal of the Royal College of General Practitioners 31, 548–552. Horsley, R.A., 2003, Jesus and empire: The Kingdom of God and the new world disorder, Fortress, Minneapolis, MN. Horsley, R.A., 2008a, ‘Jesus and Empire’, in R.A. Horsley (ed.), In the shadow of Empire: reclaiming the Bible as a history of faithful resistance, pp. 75−96, Westminster John Knox, Louisville, KY/London. Horsley, R.A., 2008b, ‘“My name is Legion”: Spirit possession and exorcism in Roman Palestine’, in F. Flannery, C. Shantz & R.A. Werline (eds.), Experientia, volume 1: Inquiry into religious experience in Early Judaism and Christianity, pp. 41−57, Society of Biblical Literature, Atlanta, GA. Hughes, C.C., 1985, ‘Culture-bound or construct-bound? The syndromes and DSM-III’, in R.C. Simons & C.C. Hughes (eds.), The culture-bound syndromes: Folk illnesses of psychiatric and anthropological interest, pp. 3−24, Reidel, Dordrecht. Inhorn, M.C., 2010, ‘Medical anthropology at the intersections: celebrating 50 years of interdisciplinarity’, Medical Anthropology Quarterly 24(2), 263–269.
doi: 10.1111/j.1548-1387.2010.01100.x Klancher, N., 2009, ‘Review of Capps, D Jesus the village psychiatrist’, Journal for the Study of the Historical Jesus 7, 199–200.
doi: 10.1163/174551909X447392 Kleinman, A., Eisenberg, L. & Good, B., 1978, ‘Culture, illness, and care: Clinical lessons from anthropologic and cross-cultural research’, Annals of Internal Medicine 88, 251–258. Kleinman, A. & Sung, L.H. (eds.), 1979, ‘Why do indigenous practitioners successfully heal?’ Social Science and Medicine 130, 7–26. Kleinman, A., 1980, Patients and healers in the context of culture: An exploration of the borderland between Anthropology, medicine, and psychiatry, University of California Press, Berkeley, CA/Los Angeles, CA/London. Kleinman, A., 1986a, ‘Concepts and a model for the comparison of medical systems as cultural systems’, in C. Currer & M. Stacey (eds.), Concepts of health, illness and disease: A comparative perspective, pp. 29−47, Berg, New York. Kleinman, A., 1986b, ‘Some uses and misuses of the social sciences in medicine’, in D.W. Fiske & R.A. Shweder (eds.), Metatheory in social science: Pluralisms and subjectivities, pp. 222−245, University of Chicago Press, Chicago, IL/London. Kriel, J.R., 1997, ‘Transforming medicine’s clinical method: A critical assessment of the influence of the natural science world-view on medicine’, Scriptura 61(2), 179–192. Kriel, J.R. 2002, ‘Patients, pills and positivism: Transforming positivistic science’, in C.W. du Toit (ed.), Brain, mind and soul: Unifying the human self, pp. 99–134 Unisa, Pretoria. Krippner, S. & Achterberg, J., 2000, ‘Anomalous healing experiences’, in E. Cardeña, S.J. Lynn & S. Krippner (eds.), Varieties of anomalous experience: Examining the scientific evidence, pp. 353−395, American Psychological Association, Washington, DC.
doi: 10.1037/10371-011 Krippner, S., 1997a, ‘Dissociation in many times and places’, in S. Krippner & S.M. Powers (eds.), Broken images, broken selves: Dissociative narratives in clinical practice, pp. 3−40, Brunner/Mazel, Washington, DC. Krippner, S., 1997b, ‘The varieties of dissociative experiences’, in S. Krippner & S.M. Powers (eds.), Broken images, broken selves: Dissociative narratives in clinical practice, pp. 336−361, Brunner/Mazel, Washington, DC. Lett, J., 1987, The human enterprise: A critical introduction to anthropological theory, Westview Press, Boulder, CO. Lock, M. & Scheper-Hughes, N., 1990, ‘A critical-interpretive approach in medical anthropology: Rituals and routines of discipline and dissent’, in T.M. Johnson & C.F. Sargent (eds.), Medical anthropology: Contemporary theory and method, pp. 47−72, Praeger, New York. Moerman, D.E., 2002, Meaning, medicine and the ‘placebo effect’, Cambridge University Press, Cambridge. Morris, D.B., 1997, ‘Placebo, pain, and belief: A biocultural model’, in A. Harrington (ed.), The placebo affect: an interdisciplinary exploration, pp. 187−207, Harvard University Press, Cambridge, MA. Murdock, G.P., 1980, Theories of illness: A world survey, University of Pittsburgh Press, Pittsburgh, PA. Pfifferling, J.-H., 1981, ‘A cultural prescription for medicocentrism’, in L. Eisenberg & A. Kleinman (eds.), The relevance of social science for medicine, pp. 197−222, D Reidelm, Dordrecht. Pilch, J.J., 1991, ‘Sickness and healing in Luke-Acts’, in J.H. Neyrey (ed.), The social world of Luke-Acts: Models for interpretation, pp. 181−209, Hendrickson, Peabody, MA. Pilch, J.J., 2000a, Healing in the New Testament: Insights form medical and Mediterranean anthropology, Fortress, Minneapolis, MN. Pilch, J.J., 2000b, ‘Improving Bible translation: the example of sickness and healing’, Biblical Theology Bulletin 30, 129–134.
doi: 10.1177/014610790003000403 Pilch, J.J., 2008, ‘The usefulness of the meaning response concept for interpreting translations of healing accounts in Matthew’s gospel’, in D. Neufeld (ed.), The social sciences and biblical translation, pp. 97−108, SBL, Atlanta, GA. Pilch, J.J., 2010, ‘Jesus’s healing activity: Political acts?’ in D. Neufeld & R.E. DeMaris (eds.), Understanding the social world of the New Testament, pp. 147−155, Routledge, London/New York. Rhodes, L.A., 1990, ‘Studying biomedicine as a cultural system’, in T.M. Johnson & C.F. Sargent (eds.), Medical anthropology: Contemporary theory and method, pp. 159–165, Praeger, New York. Singer, M., 1990, ‘Reinventing medical anthropology: toward a critical realignment’, Social Science and Medicine 30(2), 179–187.
doi: 10.1016/0277-9536(90)90078-7 Spiro, H., 1997, ‘Clinical reflections on the placebo phenomenon’, in A. Harrington (ed.), The placebo affect: An interdisciplinary exploration, pp. 37−55, Harvard University Press, Cambridge, MA. Ward, C.A., 1989, ‘The cross-cultural study of altered states of consciousness and mental health’, in C. A. Ward (ed.), Altered states of consciousness and mental health: A cross-cultural perspective, pp. 15−35, Sage, London. Wax, R. & Wax, M., 1962, ‘The magical world view’, Journal for the Scientific Study of Religion 1, 179–188.
doi: 10.2307/1384696 Weiner, H. & Fawzy, I.F., 1989, ‘An integrative model of health, disease, and illness’, in S. Cheren (ed.), Psychosomatic medicine: Theory, physiology, and practice, vol. I, pp. 9−44, International Universities Press, Madison, WI. WHO, n.d.(a), Chronic diseases, viewed 29 June
2009, from www.who.int/topics/chronic_diseases/en/index.html. WHO, n.d.(b), Surveillance of noncommunicable disease risk factors,
viewed 29 June 2009,
from www.who.int/mediacentre/factsheets/fs273/en/index.html Winkelman, M., 2009, Culture and health: Applying medical anthropology, Jossey-Bass, San Francisco, CA. Worsley, P., 1982, ‘Non-western medical systems’,
Annual Review of Anthropology 11, 257–285.
doi: 10.1146/annurev.an.11.100182.001531
|